A sugar-based response in the lungs caused by invading influenza viruses can act as a signal for when a patient has a severe risk of dying, according to an international team led by University of Alberta glycomics researchers.
The researchers are now envisioning a new set of targets that could help flatten flu mortality rates and have implications for halting future pandemics.
“We care about flu pandemics because people die,” said Lara Mahal, Canada Excellence Research Chair in Glycomics and chemistry professor in the Faculty of Science. “Especially right now with COVID-19 and the death rate. If it was like the common cold and we all got sick but recovered, it wouldn’t be such a big deal to us as it is right now.”
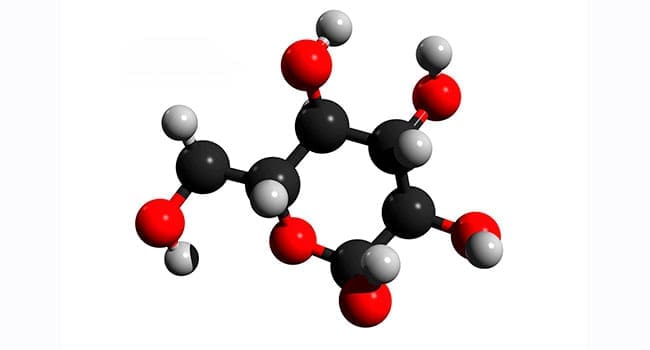
In a pair of glycomics papers published this month in The Proceedings of the National Academy of Sciences and the Journal of Proteome Research, Mahal’s team showed that high mannose glycan, a sugar that shows up in the lungs during influenza infection, is directly correlated with death from the disease.
Unlike sugars we consume as sources of energy, glycans are a class of sugar molecules that have signalling potential to tell other cells what they are and what they’re doing. Mahal explained that high mannose glycans pop up on the surface of lung cells post-infection with the flu as part of the body’s immune response.
“We think it’s actually a danger response to the virus,” she said. “It’s our innate immune system element that recognizes this sugar.
“Basically, through this response, we are damaging ourselves through overreaction to infection.”
She added the virus requires this high mannose glycan to fold and thus activate. This sugar not only helps the virus, it also ensures that virus-infected cells are recognized by the immune system.
Here’s why you should get your flu shot every year by John Muscedere
“It’s a very cool sort of system that we think is a new mechanism of thinking about how both viruses and danger signals are detected in ourselves using sugars,” she said.
In a second study using the H1N1 virus, her team looked at whether we see this mechanism in young and old populations. The 2009 H1N1 pandemic was notoriously hard on teenagers and young adults, while young children were basically left unscathed, as were older adults, who seemed to have built-in immunity developed from previous exposures.
Mahal found that the weaned segment of her animal model population infected with H1N1 didn’t get particularly sick – mirroring trends seen in 2009 – and the cell-surface sugars they were looking for never materialized. However, older animal model populations – which, unlike older humans, hadn’t built up antibodies to H1N1 – got extremely ill. And the glycan showed up in abundance in the most severe cases.
“If we’re right and this is the critical mechanism that’s causing death from the flu, then there may be a whole new way of making drugs that don’t target the very-hard-to-target evolving virus, but instead target our response to the virus in a way that makes it so that we don’t die,” she said.
Mahal, who is also a member of the Cancer Research Institute of Northern Alberta, is working with virology researcher Tom Hobman at the Li Ka Shing Institute of Virology, as well as collaborators at New York University and the National Institutes of Health, to see whether the SARS-CoV-2 virus has this impact.
Even in cancer biology, Mahal’s group found sugars that signal whether cells are going to migrate and metastasize.
“We think that now looking at this code will unlock a whole bunch of different opportunities for medical interventions.”
Mahal said current influenza flu drugs actually target a specific type of sugar. It turns out there is an enzyme the virus uses to cleave a sugar from our cell surfaces. Most of the current flu drugs inhibit that cleavage of sugar to inhibit the flu proliferation.
She added influenza biology is actually rife with sugars, but most research is centred on one called sialic acid, which is what the influenza virus sticks to in our upper respiratory tract.
“What’s interesting about our work is that we found that in terms of severity and death, sialic acid plays no role,” she said.
And while Mahal is optimistic that eventually this may indeed turn into a druggable target, her team is only still at the hypothesis stage.
“We’re really excited because we think that this is a whole new way of thinking about flu biology, and a whole new way of thinking about making drugs to interrupt the severity of this really critical disease,” she said.
| By Michael Brown and Geoff McMaster
This article was submitted by the University of Alberta’s online publication Folio, a Troy Media content provider partner.
The views, opinions and positions expressed by columnists and contributors are the author’s alone. They do not inherently or expressly reflect the views, opinions and/or positions of our publication.